Chronic Urticaria: Causes, Autoimmune Links & Treatment

Chronic urticaria (CU), or hives that won’t quit?
It is a frustrating condition that many people struggle with.
While half of the cases have no clear cause;
About 20-40% could be linked to an underlying autoimmune issue.
This means that the body’s immune system mistakenly attacks itself, sometimes triggering hives by releasing histamine—the chemical that makes you itch and swell.
Autoimmune urticaria — what’s happening
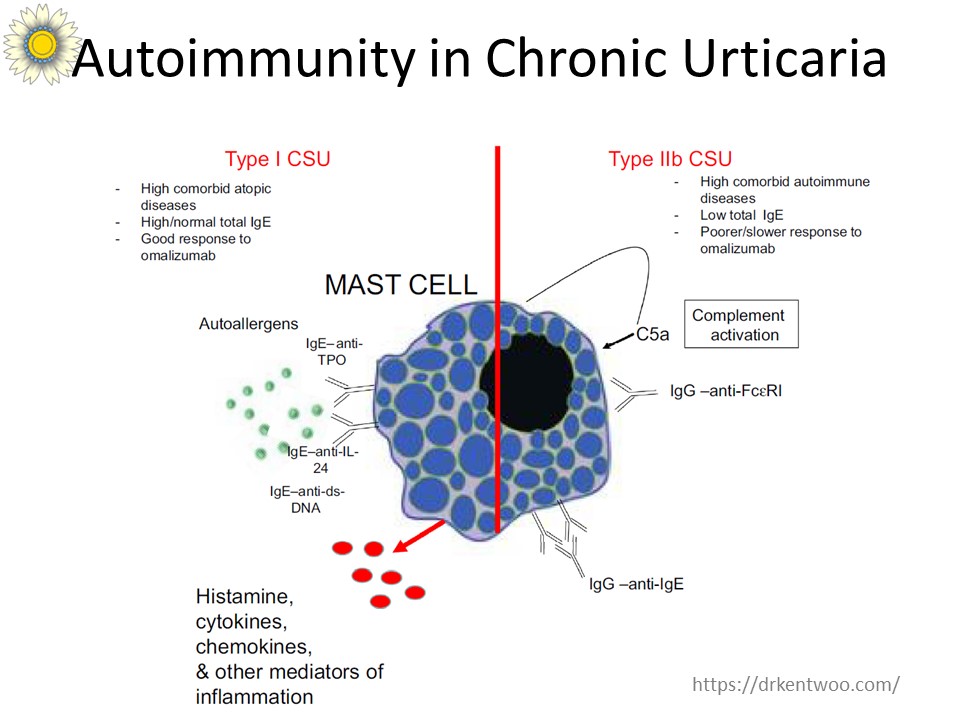
There are two simple ways your immune system can turn on you:
• Auto-IgE (autoallergy): Your body makes IgE antibodies that target your own proteins (examples: TPO, IL-24). When those IgE meet their target, mast cells release histamine → hives.
• Type IIb autoimmunity: Your body makes IgG autoantibodies that bind IgE or the IgE receptor (FcεRI) on mast cells, which also triggers histamine release.
Either route ends the same way: mast cells dump histamine and you get persistent, itchy hives.
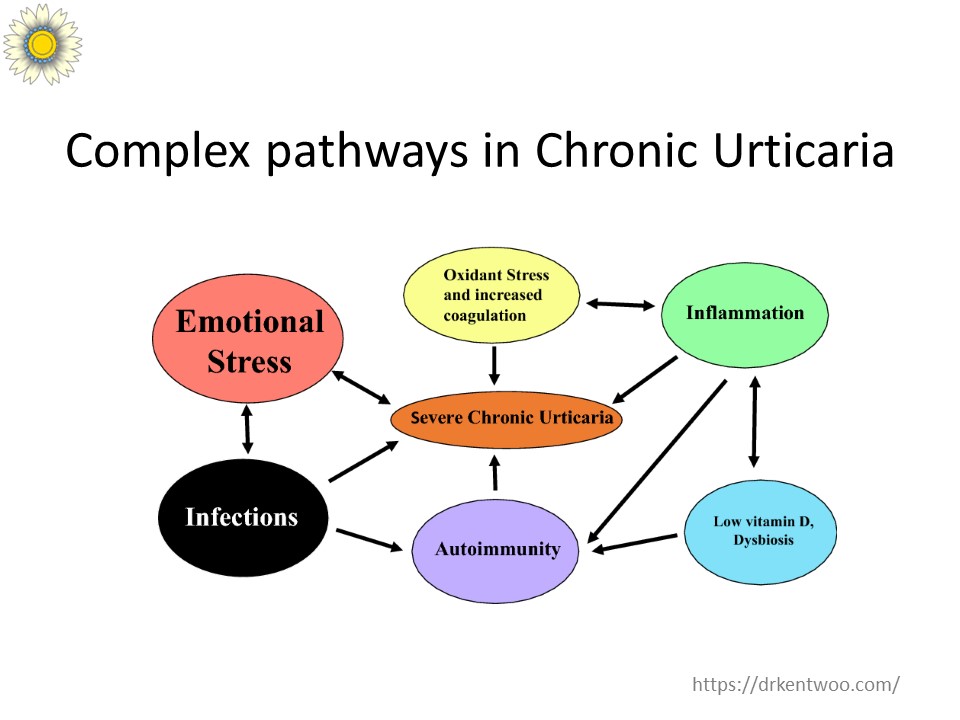
The Connection Between Chronic Urticaria and Other Autoimmune Diseases
A large study followed nearly 13,000 patients with chronic urticaria over 17 years. The results? People with chronic urticaria are more likely to develop autoimmune conditions like:
- Thyroid Issues: Both underactive and overactive thyroid, along with antibodies that mistakenly attack the thyroid gland.
- Joint Pain and Fatigue: Conditions like rheumatoid arthritis and lupus, where the immune system targets the body’s own tissues.
- Digestive Problems: Celiac disease, which is a severe reaction to gluten.
These conditions often appear within 10 years of the chronic urticaria diagnosis, so don’t shrug persistent hives off.
What to do if your hives last >6 weeks
Steps that help:
See an Allergist / Immunologist. They’ll take a targeted history and exam and may run tests (thyroid antibodies, basic autoimmune screen, or try specific investigations if indicated).
Treat the symptoms smartly. High-dose non-sedating antihistamines are the first line. If that fails, there are safe and effective next-steps (e.g., medications such as omalizumab for refractory cases).
Monitor for other autoimmune signs. New fatigue, joint pains, thyroid symptoms, or bowel changes should prompt evaluation.
🔎 Learn more: [An Unusual Treatment for Chronic Autoimmune Urticaria]
Stress & Urticaria — 5 Things That Actually Help
Stress talks to your skin — it nudges mast cells to dump histamine, and your hives flare. Try these five quick wins:
Breathe for 3–5 minutes — slow diaphragmatic breathing calms your nervous system and can reduce your stress levels.
Move gently daily — a 20–30 minute walk or yoga session lowers stress hormones and helps sleep.
Ditch late-night screens — better sleep = fewer flares. Aim for a wind-down routine.
Cut back on stimulants — reduce caffeine and booze during flare seasons; they magnify itch and anxiety.
Have a plan with your doctor — if stress triggers your hives, get a tailored action plan (antihistamine timing, or behavioral tools).
If stress feels out of control, therapy or a support group helps — and it often shows up as fewer hives, too.
When to worry
Seek urgent care if you have:
Breathing difficulty, throat tightness or dizziness (possible anaphylaxis), or
Sudden widespread swelling around the face or airway.
If you need help
If you’re dealing with chronic urticaria, don’t wait. Reach out to an Allergist/Immunologist for proper evaluation and care. The Allergy Immunology Clinic is located in Kuala Lumpur Malaysia, we are here to help you find relief.