The Practical Guide to Shrimp Allergy: Understanding, Symptoms & Management
Shrimp is one of the most common food allergens, affecting millions of people worldwide. While many are familiar with the dangers of shellfish allergies, managing them in daily life can still be challenging. Whether you’ve recently been diagnosed or have been living with shrimp allergy for years, this guide will help you understand the condition, recognize symptoms, and take practical steps to stay safe.
Understanding Shrimp Allergy
What is Shrimp Allergy?
A shrimp allergy occurs when the immune system mistakenly identifies proteins in shrimp as harmful, triggering an allergic reaction. This reaction can range from mild itching to severe, life-threatening anaphylaxis. Since shrimp is part of the crustacean family, those allergic to shrimp are often advised to avoid other shellfish, such as crabs and lobsters.
Why is Shrimp Allergy More Common in Adults Than Children?
Unlike milk or egg allergies, which children often outgrow, shrimp allergy tends to persist into adulthood. In fact, it is more commonly diagnosed in adults than in children. This is likely due to increased exposure—many people don’t consume shrimp frequently during childhood, but as they grow older and try more diverse foods, their immune system encounters shrimp proteins for the first time, potentially triggering an allergic response.
The Key Allergen: Tropomyosin and Other Shrimp Proteins
Tropomyosin is the most well-known allergen responsible for shrimp allergy. However, research has identified other proteins that can also trigger allergic reactions, including:
- Arginine Kinase: An enzyme involved in muscle energy metabolism. It has been linked to cross-reactivity between shrimp and other invertebrates like insects.
- Myosin Light Chain: A protein involved in muscle contraction, which may explain why some people react to multiple shellfish species.
- Sarcoplasmic Calcium-Binding Protein: A heat-stable allergen found in shrimp, crab, and crayfish. Because it withstands cooking, allergic reactions can still occur even when shrimp is fully cooked.
Recognizing the Symptoms
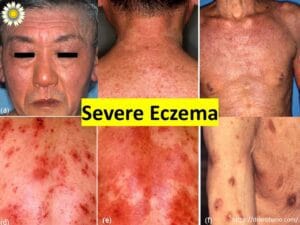
Mild to Moderate Symptoms

Mild symptoms usually develop within minutes to an hour after eating shrimp. These can include:
✔️ Itching or tingling in the mouth, lips, or throat.
✔️ Red, itchy skin rashes (hives or urticaria).
✔️ Swelling of the lips, face, or eyelids.
✔️ Stomach pain, nausea, or vomiting.
Severe Reactions (Anaphylaxis & Respiratory Distress)
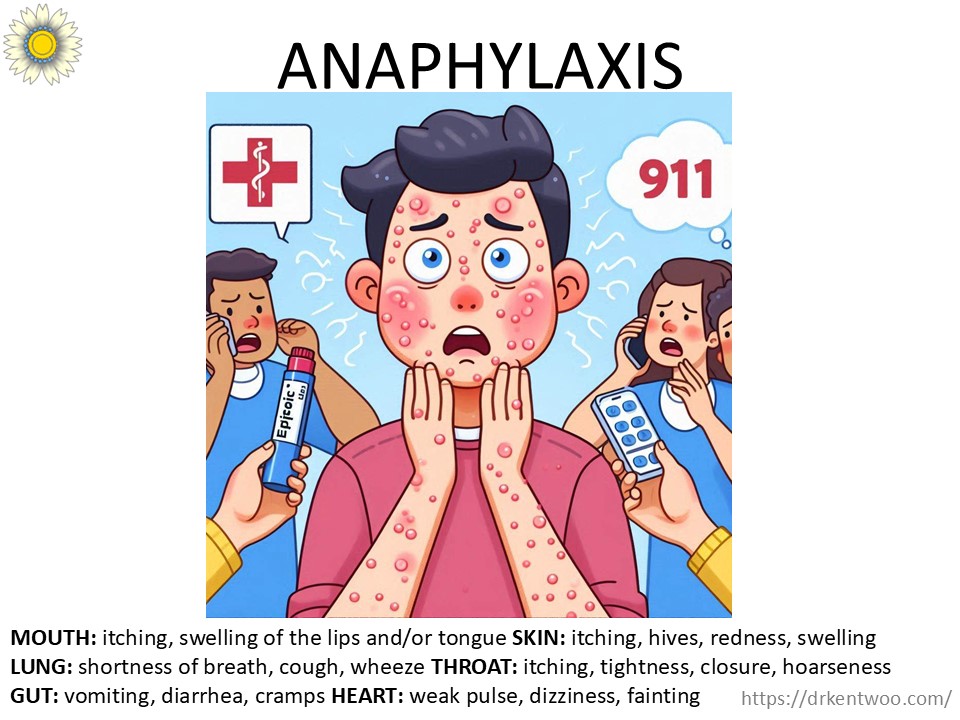
In severe cases, shrimp allergy can lead to anaphylaxis—a life-threatening reaction that requires immediate medical attention. Symptoms include:
🚨 Difficulty breathing or wheezing.
🚨 Throat swelling or a feeling of tightness in the chest.
🚨 Rapid drop in blood pressure (dizziness, fainting).
🚨 Loss of consciousness.
How Soon After Eating Shrimp Do Symptoms Appear?
Most allergic reactions to shrimp happen within minutes to an hour after consumption. However, delayed reactions can also occur, particularly in cases of mild stomach upset or skin reactions.
If you experience any severe symptoms, use an epinephrine auto-injector (EpiPen) immediately and seek emergency medical care.
Managing Shrimp Allergy in Daily Life
1. Get Evaluated by an Allergy Specialist
If you suspect you have a shrimp allergy, consult a board-certified allergist. They may conduct skin prick tests, blood tests, or an oral food challenge to confirm the diagnosis and assess cross-reactivity with other shellfish.
2. Be Aware of Cross-Reactivity
If you’re allergic to shrimp, does that mean you’re allergic to all shellfish? Not necessarily! Studies suggest:
📌 A 40% chance of reacting to other crustaceans (crab, lobster).
📌 A 15% chance of reacting to mollusks (clams, mussels, squid).
Want to know if you can eat other shellfish? Read our post on cross-reactivity between shellfish.
3. Avoid Hidden Sources of Shrimp
Shrimp can be found in unexpected places, including:
❌ Asian sauces (fish sauce, oyster sauce, shrimp paste).
❌ Processed foods (soups, bouillon, surimi, imitation seafood).
❌ Fried foods (cross-contamination in shared oil).
For a complete list of hidden sources, check out our guide on avoiding shellfish.
4. Dining Out Safely
🚨 Always inform restaurant staff about your allergy. Many kitchens use shared utensils and cooking surfaces, leading to cross-contact.
✅ Ask if the dish is prepared in the same fryer or grill as shrimp.
✅ Be extra cautious in seafood restaurants, sushi bars, and Asian cuisine establishments.
5. Carry Emergency Medication
Every person with a shrimp allergy should have an epinephrine auto-injector (EpiPen) readily available. In case of accidental exposure:
1️⃣ Inject epinephrine immediately if you develop severe symptoms.
2️⃣ Call 911 or go to the nearest hospital.
3️⃣ Take antihistamines to relieve mild symptoms, but do not rely on them alone for severe reactions.
Final Thoughts
Living with a shrimp allergy can be challenging, but with proper knowledge and preparation, you can stay safe and continue to enjoy a fulfilling diet.
✔ Learn about cross-reactivity: Can I eat other shellfish if I’m allergic to shrimp?
✔ Avoid hidden sources of shrimp: How to avoid shellfish allergy triggers
✔ Always carry emergency medication and schedule a consult with the Allergy Immunology Clinic for personalized advice.
By staying informed and proactive, you can confidently navigate your shrimp allergy and minimize the risk of reactions. Stay safe, and remember—you are not alone in this journey!