Childhood Wheeze and Asthma — A Guide from an Asthma Specialist in Malaysia

I hear this a lot in clinic.
“Ah Boy is coughing again.”
“My little girl keeps me up at night with her cough.”
These little ones are usually around 3 years old, sometimes even younger. They start kindergarten and the pattern begins: sore throat, runny nose, fever — then cough.
One parent told me her son makes a strange whistling sound — “eeeee” — when he breathes out. Another said her daughter develops coughing fits every time she runs around playing.
After a quick Google search, parents start to worry: “Could this be asthma?”
Sound familiar? If your child has repeated coughs and wheeze after viral infections, you’re not alone. As an asthma specialist in Malaysia, I see this story almost every week — worried parents, puzzled by why their child keeps coughing and wheezing.
Two Sides of Asthma: The Silent and The Loud
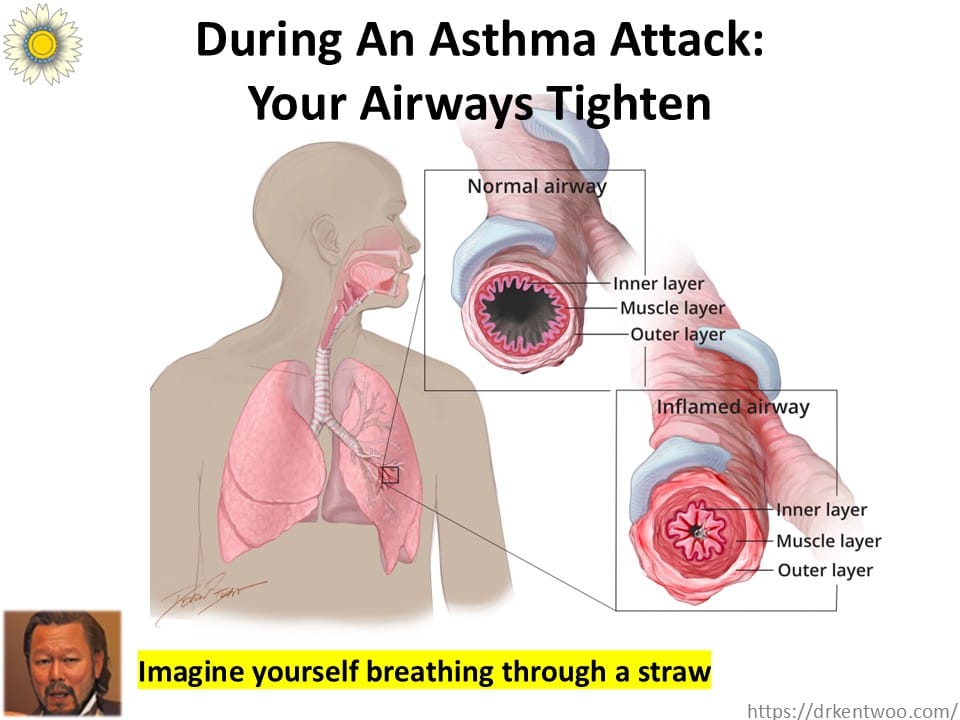
Think of asthma as two processes happening together:
The silent part: ongoing inflammation in the airways.
The loud part: airway constriction (that whistling wheeze you hear).
Inflammation makes the airways twitchy. When triggered — by cold air, infections, or smoke — they narrow and produce wheeze.
Bronchodilators help in the moment (they open up the airways quickly). But inhaled steroids treat the inflammation, lowering the chance of repeat flare-ups.
Why Kids Wheeze After Infections
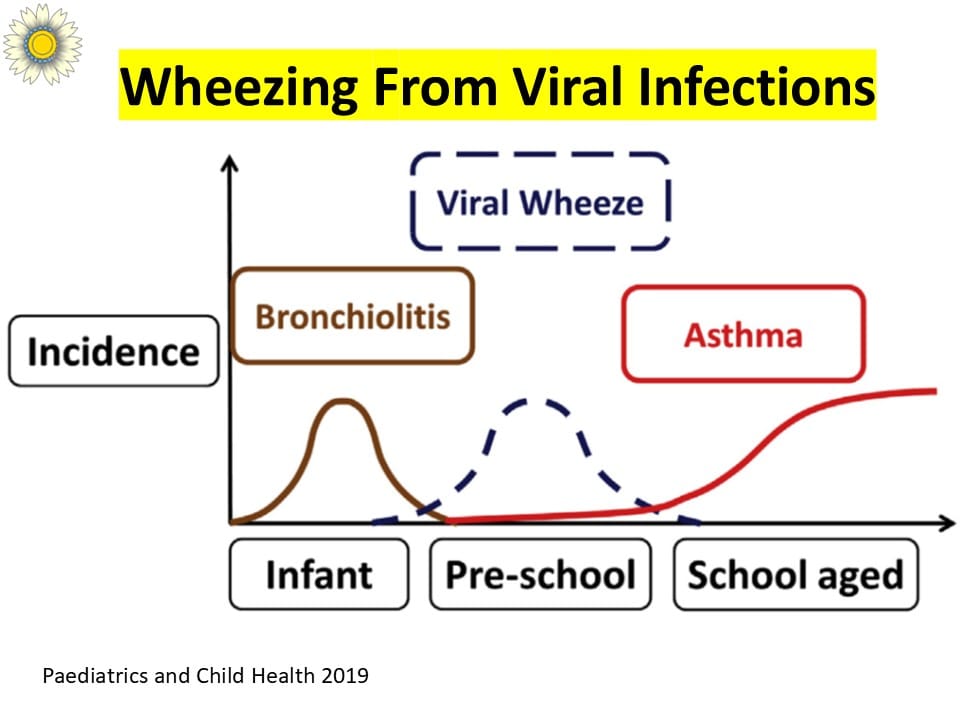
Respiratory infections are one of the most common triggers of wheeze in children.
Here’s the usual cycle:
Virus → bad cough + wheeze → recovery → repeat at the next infection.
But — and this is important — not every child who wheezes after infections will grow up to have asthma. That’s where prediction tools come in.
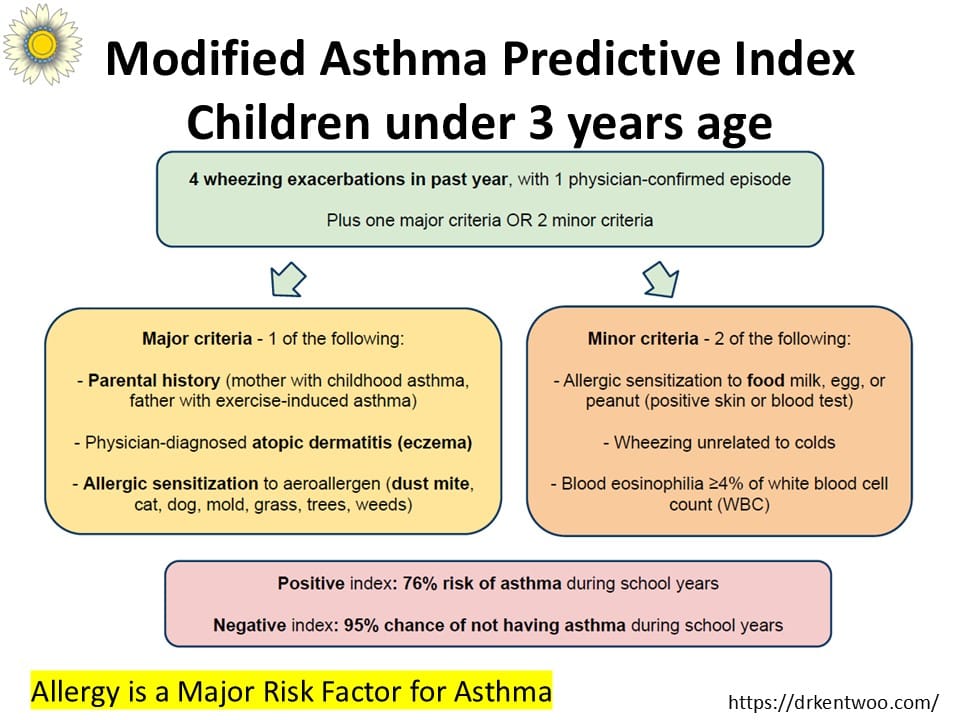
The Asthma Predictive Index (API)
Parents often ask me: “Will my child definitely have asthma when they’re older?”
We don’t have a crystal ball. But we do have the Asthma Predictive Index (API) — a clinical tool to estimate risk.
Here’s how it works:
If a child under 3 has multiple wheezing episodes plus certain risk factors (like a parent with asthma, eczema, or allergic sensitization), the chance of developing persistent asthma later is higher.
If the API is negative, many children outgrow their wheeze.
If the API is positive, the risk of asthma is higher, and we keep a closer eye.
The API isn’t perfect, but it’s simple, useful, and helps families understand the “bigger picture.”
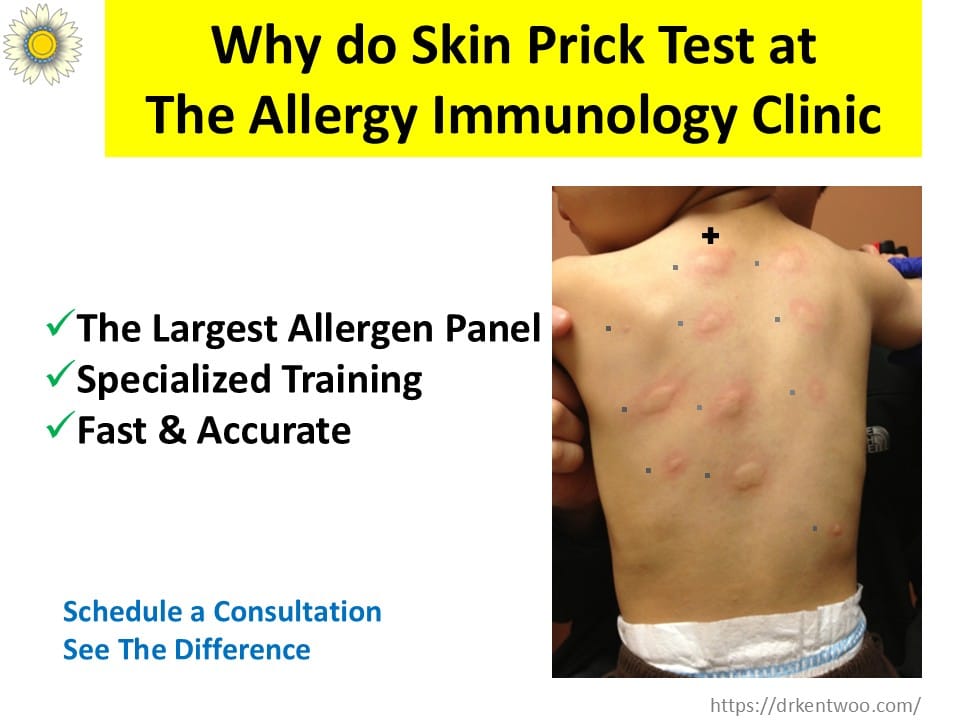
The Allergy Connection — Why Testing Matters

Here’s the part many parents don’t know: allergies play a huge role in asthma risk.
That’s why an allergy skin prick test is so valuable in children with frequent wheeze. If we find allergic sensitization — say to dust mites, cats, or pollens — the likelihood of persistent asthma is much higher.
And if we catch it early, we can:
✔ Make changes at home (dust mite covers, air filters).
✔ Choose the right preventive treatment.
✔ Even consider allergen immunotherapy — the only treatment that modifies the long-term course of allergic disease, not just symptoms.
What Parents Should Know
- You’re not failing as a parent if your child wheezes.
- Many children wheeze in preschool and grow out of it.
- Others develop persistent asthma — and that’s where early care with an asthma specialist in Malaysia makes all the difference.
With careful follow-up, smart use of inhaled steroids, and allergy testing when appropriate, we can keep children healthier, reduce flare-ups, and even change the long-term outlook.
When to See an Asthma Specialist in Malaysia
It’s a good idea to get your child checked if they have:
- Wheeze with most viral infections
- Night coughs that keep them awake
- A family history of asthma, eczema, or allergies
- Reactions to triggers at home (dust mites, pets, mold)
At The Allergy Immunology Clinic, we combine modern asthma treatment with allergy testing and immunotherapy to give children the best chance at a healthier future.
📅 Book a consultation today and let’s figure out whether it’s just “a cough” — or something we can manage better, together.